Urothelial cancer refers to cancer of the lining of the urinary system and is most common in the bladder (rather than the kidney or ureter). The modern, standard evaluation of a patient with suspicion of urothelial cancer involves axial imaging of the upper tract and bladder with an associated cystoscopy and urinary cytology. A number of tests have been developed to supplant or act as adjuncts to the standard urothelial bladder cancer evaluation. However, the current regimen of cystoscopy and urine cytology will detect 90% of urothelial bladder cancers. This blog will review some of the common alternative urinary markers for bladder cancer used in practice.
Urinary cytology is the microscopic examination of cells found in the urine. Cytology was first developed by Papanicolaou in 1945 and remains the gold standard urine test for the evaluation of suspected malignancy. The sensitivity (meaning a negative test rules out disease) ranges from 40-60%, however the specificity (a positive test indicates cancer) is high, ranging from 94-100%. The sensitivity and specificity of a urinary cytology depends on the tumor grade, tumor stage, the number of samples evaluated and the experience of the cytopathologist who evaluates the sample. In addition, instrumented samples (i.e. from a bladder wash during cystoscopy) have a higher yield and better sensitivity that voided urine.[1]
 |
| Urinary cytology demonstrating cancer cells. From http://www.pathologypics.com/PictView.aspx?ID=106 |
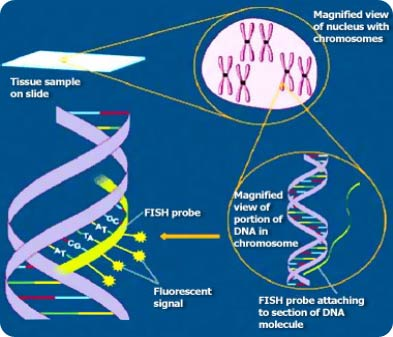
FISH stands for Fluorescence in situ Hybridization and refers to a technique where fluorescently-labeled DNA probes are designed to bind to intranuclear chromosomes (the genetic material of cells). While they can be used for a variety of cancers, FISH probes have been developed to look for common genetic abberations in bladder cancer including aneuploidy of chromosomes 3, 7, 17 and homozygous loss of 9p21.
Compared to urinary cytology, the sensitivity and specifity are 79% and 70% respectively. FISH is highly dependent on an experienced laboratory to process and interpret the results of each test, however has been demonstrated to have a sensitivity dramatically improved when compared to urinary cytology. Importantly, the sensitivity of FISH improves with increasing grade and stage of bladder tumors. In some patients, FISH can provide confidence that no cancer is present. However, false positive tests are relatively common and may indicate a “precurrence” of cancer or genetic abnormalities that exist in the normal urothelium. The role of FISH in the everyday management of bladder cancer is not well-defined and utility may vary by practitioner.[2-4]
NMP-22 (Nuclear Matric Protein) is a molecule preferentially shed into the urine by bladder cancer cells to that NMP22 levels are, on average, 20x higher in patients with bladder cancer than those without cancer. Unfortunately, the cutoff values for an abnormal NMP22 are not well established and a higher NMP22 level does not correlate to worse grade or stage of disease. The sensitivity and specificity of NMP22, using a cutoff of 10units/mL, are reported to be 49% and 87% respectively. The sensitivity does improve for higher stage tumors. However, false positives have been noted in patients with active urinary tract infections and hematuria.[5-7]
A number of other promising markers are in development but are not clinically available for most patients. These include tests like Lewis Blood Group Antigen X which is absent in normal cells and present in urothelial cancer cells of the bladder.[8] CK20 and CYFRA21.1 are proteins found in the cytoskeleton of bladder cancer cells and can be detected by protein or RNA analysis of the urine.[9] Metabolomics is a promising avenue for discovery, where metabolites in the urine can vary between patients with and without cancer. Preliminary studies demonstrate varying metabolite patterns for patients with and without cancer, however no test has proven superior to cystoscopy and cytology as of yet.
[1] Volpe A, Racioppi M, D'Agostino D, Cappa E, Gardi M, Totaro A, Pinto F, Sacco E, Marangi F, Palermo G, Bassi PF. Bladder tumor markers: a review of the literature. Int J Biol Markers. 2008 Oct-Dec;23(4):249-61.
[2] Sarosdy MF, Schellhammer P, Bokinsky G, Kahn P, Chao R, Yore L, Zadra J, Burzon D, Osher G, Bridge JA, Anderson S, Johansson SL, Lieber M, Soloway M, Flom K. Clinical evaluation of a multi-target fluorescent in situ hybridization assay for detection of bladder cancer. J Urol. 2002 Nov;168(5):1950-4.
[3] van Rhijn BW, van der Poel HG, and van der Kwast TH: Urine markers for bladder cancer surveillance: a systematic review. Eur Urol 2005; 47: pp. 736-748
[4] Yoder BJ, Skacel M, Hedgepeth R, et al: Reflex UroVysion testing of bladder cancer surveillance patients with equivocal or negative urine cytology: a prospective study with focus on the natural history of anticipatory positive findings. Am J Clin Pathol 2007; 127: pp. 295-301
[5] Atsu N, Ekici S, Oge OO, et al: False-positive results of the NMP22 test due to hematuria. J Urol 2002; 167: pp. 555-558
[6] Grossman HB, Soloway M, Messing E, et al: Surveillance for recurrent bladder cancer using a point-of-care proteomic assay. JAMA 2006; 295: pp. 299-305
[7] Keesee SK, Briggman JV, Thill G, and Wu YJ: Utilization of nuclear matrix proteins for cancer diagnosis. Crit Rev Eukaryot Gene Expr 1996; 6: pp. 189-214
[8] Sheinfeld J, Reuter VE, Melamed MR, et al: Enhanced bladder cancer detection with the Lewis X antigen as a marker of neoplastic transformation. J Urol 1990; 143: pp. 285-288
[9] Ramos D, Navarro S, and Villamon R: Cytokeratin expression patterns in low-grade papillary urothelial neoplasms of the urinary bladder. Cancer 2003; 97: pp. 1876-1883